10 Body Systems Every Nurse Should Master
Nov 25, 2025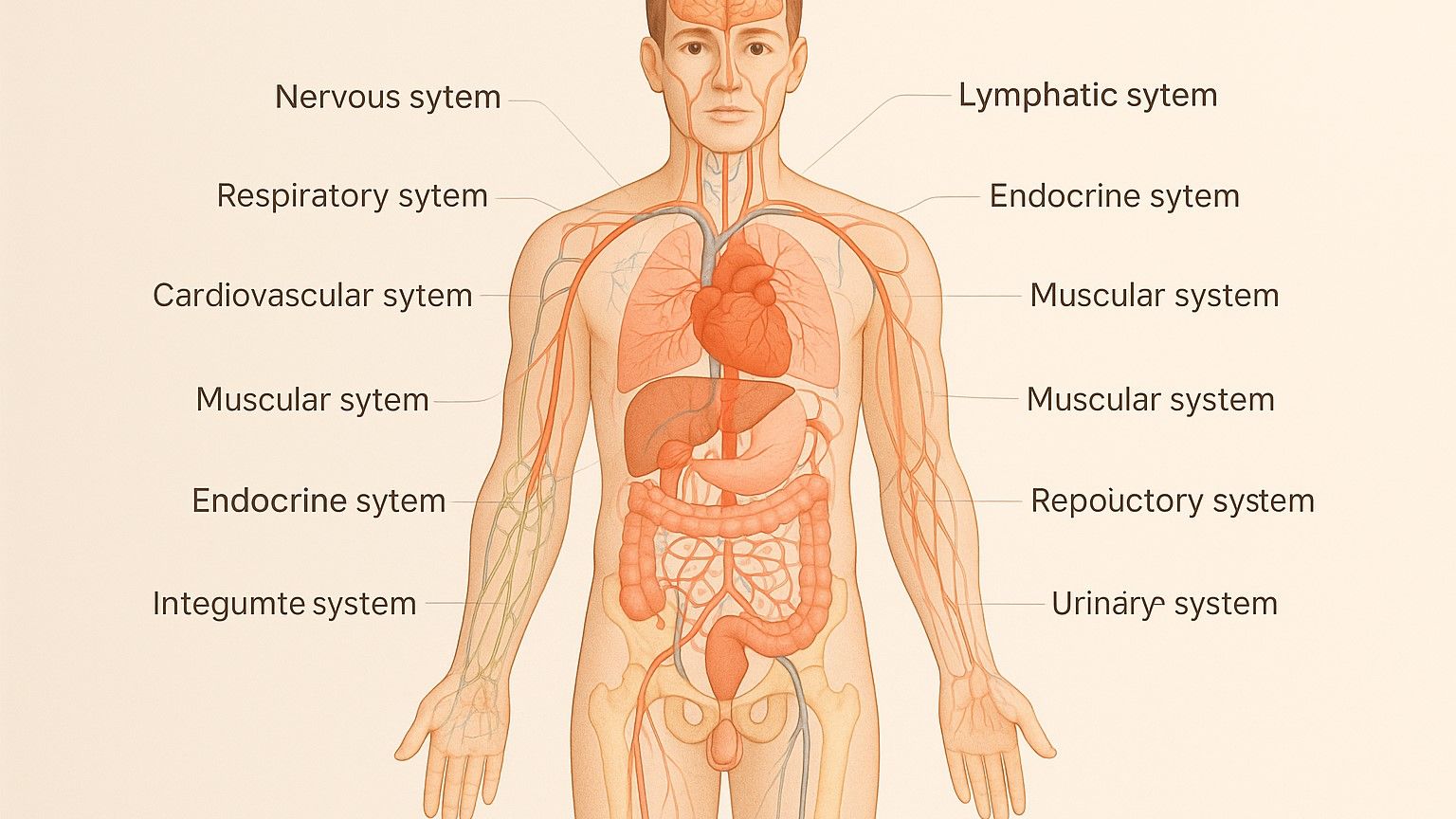
Nurses need a strong understanding of the body's systems to provide safe and effective care. From spotting early signs of emergencies like strokes or heart attacks to managing chronic conditions like diabetes, this knowledge is essential. Here’s a quick breakdown of the 10 key systems every nurse should know:
- Circulatory System: Focuses on blood flow, heart rhythms, and blood pressure. Key for managing conditions like heart failure and hypertension.
- Respiratory System: Involves breathing mechanics, oxygen levels, and lung function. Essential for treating issues like asthma or respiratory distress.
- Muscular System: Supports movement and stability. Important for handling conditions like osteoarthritis and muscle injuries.
- Skeletal System: Provides the body's structure and protects organs. Nurses monitor for fractures, osteoporosis, and arthritis.
- Nervous System: Controls body functions and responses. Critical in stroke care, seizure management, and spinal injuries.
- Digestive System: Processes food and nutrients. Nurses address issues like acid reflux, constipation, and GI disorders.
- Urinary System: Filters waste and manages fluid balance. Key for monitoring kidney function and managing UTIs.
- Endocrine System: Regulates hormones affecting growth, metabolism, and stress. Central to managing diabetes and thyroid issues.
- Integumentary System: Includes skin, hair, and nails. Nurses assess wounds, infections, and pressure injuries.
- Reproductive System: Covers male and female reproductive health. Important for addressing conditions like infertility and reproductive cancers.
These systems work together, and nurses must understand how changes in one can affect others. This interconnected knowledge helps improve patient outcomes and ensures better communication with healthcare teams.
NCLEX-RN/PN Body Systems Study Guide
1. Circulatory System
The circulatory system plays a vital role in the body by transporting oxygen, nutrients, and hormones while removing waste products. For nurses, a solid grasp of this system is essential for identifying and managing circulatory disorders in clinical settings.
To start, understanding the heart's anatomy is key. The heart has four chambers: the right atrium and ventricle and the left atrium and ventricle. Blood flows through these chambers in a specific sequence. The right atrium receives deoxygenated blood from the body, which the right ventricle then pumps to the lungs for oxygenation. From there, the oxygen-rich blood enters the left atrium and is pumped by the left ventricle to the rest of the body. This knowledge helps nurses detect abnormalities in blood flow, which can often be reflected in changes to vital signs.
Blood pressure is another critical indicator of circulatory health. Elevated systolic or diastolic readings can signal potential hypertensive crises, requiring immediate attention. By closely monitoring these numbers, nurses can intervene early to prevent complications.
Heart failure is another area where understanding the circulatory system is crucial. Left-sided heart failure often results in pulmonary congestion, leading to symptoms like shortness of breath and abnormal lung sounds. In contrast, right-sided heart failure typically causes peripheral edema. Recognizing these differences is essential for prioritizing care and communicating effectively with the healthcare team.
Peripheral circulation is equally important. Assessing for conditions like deep vein thrombosis involves checking for the "5 Ps" - pain, pallor, pulselessness, paresthesia, and paralysis. These signs can indicate compromised circulation and require swift action to prevent further complications.
Medications such as ACE inhibitors (e.g., lisinopril) and beta-blockers (e.g., metoprolol) directly affect circulation. Nurses must monitor patients closely for side effects and provide clear education about these treatments to ensure safety and adherence.
Cardiac monitoring is another critical skill, requiring an understanding of the heart's electrical conduction system. From the sinoatrial node to the atrioventricular node, bundle of His, and Purkinje fibers, this system controls heart rhythms. Detecting arrhythmias like ventricular tachycardia or atrial fibrillation can be life-saving.
Lastly, the circulatory system’s interaction with other body systems adds complexity to patient care. For example, fluid balance impacts blood volume and pressure, while kidney and respiratory function are closely tied to circulatory stability. A deep understanding of these connections equips nurses to provide comprehensive care and respond effectively to changes in a patient’s condition.
2. Respiratory System
The respiratory system is the cornerstone of life, delivering oxygen to the body and removing carbon dioxide. Any disruption in its function can rapidly become life-threatening, making its proper assessment and care a top priority.
To understand respiratory function, it's critical to know the anatomy of the respiratory tract. The upper tract includes the nose, mouth, pharynx, and larynx, while the lower tract consists of the trachea, bronchi, bronchioles, and alveoli. Clinical signs often point to specific issues: for example, stridor signals an obstruction in the upper airway, while wheezing points to lower airway conditions like asthma or chronic obstructive pulmonary disease (COPD).
Breathing rates vary by age: adults typically breathe 12–20 times per minute, while infants breathe faster at 30–60 times per minute. Abnormal patterns can reveal underlying problems. Tachypnea (rapid breathing) might indicate respiratory distress, infection, or pain, whereas bradypnea (slow breathing) could suggest central nervous system depression - often from medications like opioids - or neurological conditions.
Monitoring oxygen saturation has become standard practice. Normal levels fall between 95–100%, but patients with COPD often have a baseline of 88–92%. Over-oxygenating these patients can suppress their respiratory drive, so careful management is essential to avoid unintended harm.
Breath sounds are another key diagnostic tool. Normal vesicular sounds should be clear and equal on both sides. Abnormal sounds provide important clues:
- Crackles (rales): Often caused by fluid in the alveoli, as seen in heart failure or pneumonia.
- Rhonchi: Suggest secretions in the larger airways.
- Diminished or absent sounds: May point to conditions like pneumothorax or pleural effusion.
These findings guide immediate interventions and help prioritize care.
Breathing mechanics also reveal a lot about respiratory health. Inspiration occurs when the diaphragm contracts and intercostal muscles lift the ribs, while expiration happens passively through elastic recoil. When patients use accessory muscles to breathe, it’s often a sign of increased effort and potential respiratory compromise.
The respiratory system also plays a critical role in maintaining acid-base balance. The lungs regulate pH by controlling carbon dioxide levels. Hyperventilation, which blows off excess CO2, can lead to respiratory alkalosis, while hypoventilation causes CO2 retention, resulting in respiratory acidosis. Understanding these processes is vital when interpreting arterial blood gas results and assessing the body’s compensatory mechanisms.
Medications for respiratory conditions require careful attention. For instance:
- Bronchodilators like albuterol can cause side effects such as tachycardia and tremors.
- Corticosteroids like prednisone may increase blood glucose levels.
Teaching patients proper inhaler techniques ensures they get the full benefit of their medications.
Positioning can significantly improve breathing for patients in distress. Elevating the head using the semi-Fowler’s position (30–45 degrees) or high-Fowler’s position (60–90 degrees) can ease respiratory effort. Prone positioning, widely used during the COVID-19 pandemic, has also been shown to enhance oxygenation in many cases.
The respiratory system's connection to other body systems adds layers to patient care. Respiratory infections, for example, can quickly lead to sepsis, affecting multiple organs. Neuromuscular disorders may weaken respiratory muscles, sometimes requiring ventilatory support. Recognizing these interconnections allows nurses to anticipate complications and provide well-rounded care.
In cases of respiratory arrest, immediate action is critical. This includes providing bag-mask ventilation, assisting with intubation, and managing ventilators. Next, let’s explore how the muscular system contributes to respiratory function and overall health.
How Does Breathing Actually Work???
3. Muscular System
The muscular system is essential for movement and stability. For nurses, understanding how muscles work is key to identifying and managing musculoskeletal conditions like osteoarthritis. While osteoarthritis primarily affects the joints, it can also hinder muscle performance and reduce a patient’s mobility.
When caring for patients with osteoarthritis, nurses can take several steps to provide relief and improve comfort:
- Use ice or heat during flare-ups to ease pain.
- Apply prescribed topical treatments.
- Reposition patients to alleviate discomfort.
- Offer gentle massages to relax muscles.
Maintaining overall musculoskeletal health is just as important. Nurses should encourage patients to engage in weight-bearing exercises to help maintain motion, flexibility, and strength. Supporting activities like walking and promoting independent movement can further enhance recovery and mobility.
Diet also plays a critical role in keeping the muscles and bones healthy. Protein-rich foods aid in tissue repair, while calcium-rich options - like dairy products, fortified plant-based milks, and leafy greens - help preserve bone health and strengthen the muscle-bone connection.
A well-functioning muscular system relies on a strong skeletal framework. Together, these systems work in harmony to support movement and stability.
4. Skeletal System
The skeletal system serves as the body's structural foundation, working hand-in-hand with the muscular system to enable movement while also protecting vital organs. For nurses, understanding this system is crucial for identifying and managing bone-related conditions early.
Osteoporosis is a common and serious condition that nurses often encounter. It weakens bones by reducing their density, making fractures more likely - especially in the hip, spine, and wrist. This condition is particularly prevalent among older women. Nurses can assess for osteoporosis through patient history, symptom evaluation, and physical exams, using tools like the PQRSTU approach and palpation.
Managing osteoporosis involves a multi-faceted strategy. Patient education is central, emphasizing a diet rich in calcium and vitamin D, regular weight-bearing exercises, and avoiding smoking, which can accelerate bone loss. For severe cases, medications such as bisphosphonates or calcitonin may be prescribed to slow bone deterioration. Care plans should also focus on safe positioning, gentle ambulation, and tailored exercises to reduce the risk of fractures while accommodating patient fragility.
Fractures demand immediate attention and careful assessment. Nurses should look for key signs such as pain, swelling, bruising, deformity, tenderness, numbness, tingling, or difficulty moving the affected area. If a fracture is suspected, prompt medical evaluation and imaging, like an X-ray, are essential. Hip fractures, for example, often cause severe pain, limited mobility, swelling, bruising, and a shortened or externally rotated leg. Treatment may range from immobilization with a cast or splint to surgical intervention using plates, pins, or screws. Post-surgery care for hip fractures includes assisting with mobility, implementing fall prevention strategies, and monitoring for complications like pneumonia, pressure injuries, or pulmonary embolism. Timely interventions can significantly improve recovery and patient outcomes.
Arthritis presents in two primary forms, each requiring distinct management approaches. Osteoarthritis, the more common type, results from aging and the gradual breakdown of cartilage in the joints. Early symptoms, such as joint pain and inflammation, may improve with light activity, but as the condition progresses, pain worsens and mobility declines. Management strategies include weight loss, low-impact exercises, and medications like acetaminophen, NSAIDs, or celecoxib. In advanced cases, joint replacement surgery may become necessary.
Rheumatoid arthritis, on the other hand, is an autoimmune disorder that causes joint pain, swelling, stiffness, and reduced function due to inflammation. It typically begins in middle age and is more common in women. By understanding both types of arthritis, nurses can create personalized care plans and provide effective patient education.
Healthy bones are the foundation for strong, stable movement, anchoring muscles and supporting the body’s overall functionality.
5. Nervous System
The nervous system is the body’s command center, orchestrating everything from basic survival functions to complex thought processes. Its health and functionality are critical in clinical care, influencing how medical teams respond to emergencies and manage patient outcomes. For nurses, having a deep understanding of this intricate system is vital for identifying neurological crises, monitoring patients, and delivering effective care.
One of the most urgent neurological conditions nurses face is a stroke. When blood flow to the brain is disrupted, every second counts. Nurses use the FAST assessment to identify stroke symptoms: Face drooping, Arm weakness, Speech difficulties, and Time to call emergency services. Additional red flags include sudden, severe headaches, confusion, vision disturbances, dizziness, and loss of coordination.
Most strokes - about 87% - are ischemic, caused by blood clots. These can often be treated with clot-dissolving medications like tPA, but only if administered within a narrow window of 3–4.5 hours. Hemorrhagic strokes, on the other hand, require immediate surgical intervention to manage bleeding. After the initial treatment, nurses play a key role in post-stroke care, monitoring for complications like increased intracranial pressure, seizures, and aspiration pneumonia. This involves tasks like positioning patients to prevent aspiration, using the Glasgow Coma Scale to assess neurological status, and coordinating rehabilitation efforts to support recovery.
Another critical area of focus is managing seizures, which demand swift action to ensure patient safety. Generalized tonic-clonic seizures involve loss of consciousness, muscle stiffness, and rhythmic jerking, while focal seizures may cause altered awareness, sensory changes, or repetitive movements without a loss of consciousness. A prolonged seizure or repeated seizures without recovery - known as status epilepticus - is a medical emergency that requires immediate intervention.
During a seizure, nurses must prioritize safety by keeping the patient’s airway clear, positioning them on their side to prevent aspiration, and removing nearby objects that could cause injury. It’s important not to place anything in the patient’s mouth or try to restrain their movements. Accurate documentation of the seizure’s duration, type, and any post-seizure behavior is essential for guiding treatment adjustments.
In cases of dementia and Alzheimer’s disease, care extends beyond physical health to address the progressive decline in memory, reasoning, and behavior. These conditions affect around 6.7 million Americans aged 65 and older. Early signs include difficulty recalling recent events, getting lost in familiar places, and trouble solving problems or completing routine tasks.
Caring for patients with dementia requires patience and adaptable communication. Speaking slowly and clearly, maintaining eye contact, and using simple language can help. Consistent routines can ease confusion and anxiety, while managing sundowning - a phenomenon where agitation increases in the late afternoon or evening - often involves structured activities, good lighting, and calming environments.
For patients with spinal cord injuries, immediate and ongoing neurological assessment is crucial to prevent further damage and support recovery. Injuries are classified as either complete, with total loss of sensation and movement below the injury, or incomplete, where some function remains. The location of the injury significantly impacts the patient’s abilities. For example, cervical injuries might impair breathing and require ventilatory support, while lumbar injuries typically affect lower body functions and bladder control.
Nurses must also watch for autonomic dysreflexia, a dangerous condition seen in patients with spinal cord injuries above the T6 level. This condition causes a sudden spike in blood pressure, often triggered by stimuli like a full bladder or pressure sores. Symptoms include severe headaches, sweating above the injury site, and slow heart rate. Promptly addressing the underlying cause is critical to managing this life-threatening situation.
Finally, traumatic brain injuries (TBI) range from mild concussions to severe, life-altering damage. Assessment often relies on the Glasgow Coma Scale, which measures eye opening, verbal responses, and motor responses, with scores ranging from 3 to 15. Lower scores indicate more severe injuries. Nurses must closely monitor for signs of increased intracranial pressure, such as changes in consciousness, pupil reactions, vital signs, and motor function.
The nervous system, with its intricate network of neurons and neurotransmitters, governs every aspect of human function. Understanding its complexities enables nurses to provide the comprehensive care needed to support patients through neurological challenges.
6. Digestive System
The digestive system handles breaking down food, absorbing nutrients, and getting rid of waste. It’s made up of the gastrointestinal (GI) tract and accessory organs that work together to keep the process running smoothly.
It all starts in the mouth, where chewing (mechanical digestion) breaks food into smaller pieces, and saliva enzymes begin the chemical breakdown. This forms a soft, swallowable mass called a bolus.
The bolus then travels through the pharynx and into the esophagus. Here, wave-like muscle movements, known as peristalsis, push the bolus downward. To prevent food from going down the wrong pipe, the epiglottis - a small flap - covers the trachea during swallowing.
At the end of the esophagus, the lower esophageal sphincter acts like a gatekeeper. It opens to let food enter the stomach but closes tightly to stop stomach contents from coming back up. This mechanism is key to understanding issues like acid reflux, which nurses often encounter.
Once in the stomach, the food undergoes further breakdown. Muscular contractions mix it with stomach acid and digestive enzymes, starting the chemical digestion process in earnest.
7. Urinary System
The urinary system plays a key role in filtering waste from the blood and maintaining the body’s fluid balance. For nurses, understanding this system is essential, as kidney and urinary issues are among the most frequent conditions encountered in clinical practice.
It all begins with the kidneys, two bean-shaped organs located just below the ribcage on either side of the spine. These organs are powerhouses, each containing about one million tiny filtering units called nephrons. Together, they process an impressive 50 gallons of blood daily, removing waste products like urea and creatinine while ensuring vital substances such as proteins and red blood cells remain in circulation. Blood enters the kidneys via the renal artery, flowing into the glomerulus - a cluster of tiny blood vessels within each nephron. Here, filtration begins as water and small molecules pass through the glomerular membrane, creating a substance called filtrate. This filtrate then travels through a network of tubules, where the body reabsorbs useful elements like glucose, sodium, and most of the water.
The ureters, two muscular tubes, carry urine from the kidneys to the bladder. They use peristaltic movements to push the urine downward, even when a person is lying flat.
The bladder acts as a storage reservoir, expanding as it fills with urine. Stretch receptors in the bladder wall signal when it’s time to empty. A healthy adult bladder can typically hold about 16-24 fluid ounces before the urge to urinate becomes noticeable.
The final step involves the urethra, which serves as the exit pathway. In females, the urethra is about 1.5 inches long, while in males, it measures around 8 inches and passes through the prostate gland. This anatomical difference explains why women are more prone to urinary tract infections - bacteria have a much shorter distance to travel.
Monitoring urine output is a critical aspect of patient care. A healthy adult produces about 1-2 liters of urine per day, or roughly 30-50 milliliters per hour. If output drops below 30 mL/hour (a condition known as oliguria), it may signal kidney problems or dehydration.
The kidneys also play a key role in regulating blood pressure through the renin-angiotensin system. When blood pressure falls, the kidneys release renin, a hormone that triggers a series of reactions to raise blood pressure and retain fluid. This is why many blood pressure medications target this system.
Another essential function of the kidneys is maintaining electrolyte balance. They regulate levels of sodium, potassium, calcium, and phosphorus to keep the body functioning properly. Lab results such as elevated creatinine or a reduced glomerular filtration rate (GFR) often point to declining kidney function and require immediate attention.
Common urinary system disorders include urinary tract infections, kidney stones, chronic kidney disease, and acute kidney injury. Each condition presents unique symptoms and requires tailored nursing interventions, such as monitoring fluid intake and output, administering medications, and educating patients about dietary adjustments. The urinary system’s ability to manage waste and fluid balance highlights its vital role in overall health and its interconnectedness with other body systems.
8. Endocrine System
The endocrine system uses hormones to manage a wide range of functions, from regulating your heart rate to controlling your sleep patterns. For nurses, understanding this system is essential because even minor hormone imbalances can have widespread effects on a patient’s health.
"The endocrine (hormonal) system is a network of glands that release hormones to regulate processes such as growth, metabolism and reproduction." – healthdirect
Unlike other systems that rely on direct connections, the endocrine system communicates through the bloodstream. Hormones, the chemical messengers of this system, travel to specific organs and tissues to trigger precise responses. Even tiny amounts can cause significant changes in the body.
At the core of the endocrine system is the hypothalamus-pituitary axis. The hypothalamus, located deep in the brain, acts as a bridge between the nervous and endocrine systems. It monitors factors like body temperature and stress levels, then sends signals to the pituitary gland - a pea-sized structure often referred to as the "master gland."
"The pituitary gland is often called the 'master gland' because it regulates many other endocrine glands." – healthdirect
The anterior pituitary releases hormones such as growth hormone and thyroid-stimulating hormone, while the posterior pituitary secretes oxytocin and antidiuretic hormone (ADH).
The thyroid gland, shaped like a butterfly and located in the neck, functions as the body’s metabolic regulator. It produces T3 and T4 hormones, which determine how quickly cells use energy. When the thyroid malfunctions, patients may experience weight changes, sensitivity to temperature, or irregular heart rhythms. Additionally, the thyroid produces calcitonin, which helps regulate calcium levels in the blood.
The four parathyroid glands, found behind the thyroid, play a key role in calcium balance through the release of parathyroid hormone (PTH). Proper calcium levels are critical for muscle contractions, nerve signaling, and bone health.
Sitting atop each kidney, the adrenal glands have two parts with distinct roles. The outer cortex produces hormones like cortisol and aldosterone, while the inner medulla releases adrenaline and noradrenaline, which are essential for the body’s stress response.
The pancreas serves dual purposes as an endocrine and digestive organ. Its endocrine cells, known as the islets of Langerhans, produce insulin and glucagon to regulate blood sugar levels. Disruptions in this balance can lead to diabetes, a condition requiring careful management.
The pineal gland, a tiny, pine-cone-shaped structure in the brain, produces melatonin, which helps regulate sleep cycles.
Reproductive glands - ovaries in females and testes in males - produce sex hormones that influence puberty, fertility, and secondary sexual characteristics.
The endocrine system depends on feedback loops to maintain hormonal balance. Most of these loops function through negative feedback, similar to a thermostat: when hormone levels are too high, production decreases, and when levels are too low, production increases. Understanding these loops is crucial for diagnosing and managing endocrine disorders.
Common conditions affecting the endocrine system include diabetes, thyroid disorders, adrenal insufficiency, and hormone imbalances related to reproduction. Each condition requires close monitoring and patient education, especially regarding lifestyle choices that promote hormonal health.
For patients on long-term corticosteroid therapy, it’s critical to avoid stopping the medication abruptly, as this can trigger a potentially life-threatening Addisonian crisis. Instead, doses must be tapered gradually to allow the adrenal glands to recover. Nurses should monitor these patients for side effects like high blood sugar, weakened bones, and an increased risk of infections.
The delicate balance of hormones underscores how interconnected the body’s systems are, setting the stage for the next discussion on the integumentary system.
9. Integumentary System
The integumentary system is the body’s largest organ system, encompassing the skin, hair, nails, and various glands. For nurses, it serves as a vital indicator of a patient’s overall health during routine assessments.
The skin is made up of three main layers, each serving a distinct purpose. The epidermis, the outermost layer, acts as a protective shield against pathogens, chemicals, and physical damage. This layer is constantly regenerating, with new cells forming at the base and moving upward over about 28 days. Beneath it lies the dermis, which houses blood vessels, nerve endings, hair follicles, and sweat glands. This layer provides structural support and contains sensory receptors that help us perceive touch, pressure, and temperature. The deepest layer, the hypodermis (or subcutaneous tissue), consists mostly of fat cells, offering insulation and cushioning for internal organs.
The integumentary system plays several critical roles in maintaining health. It helps regulate body temperature through sweat production and blood vessel dilation or constriction. It also synthesizes vitamin D when exposed to sunlight, which is essential for bone health. Additionally, the system acts as a sensory interface, allowing the body to gather information about its surroundings through touch and temperature receptors.
Hair and nails, while often seen as cosmetic features, provide valuable health insights. Changes in hair texture, growth, or loss can signal nutritional deficiencies, hormonal imbalances, or systemic illnesses. Similarly, nails can reveal underlying issues like respiratory problems, heart conditions, or infections through alterations in color, shape, or growth.
The integumentary system also includes several types of glands that are important for nurses to understand. Sebaceous glands produce oil that keeps the skin and hair moisturized. Sweat glands help regulate body temperature and eliminate some waste products. Apocrine glands, located in areas like the armpits and groin, become active during puberty and contribute to body odor when bacteria break down their secretions. These glandular functions play a key role in skin assessment and wound healing.
When assessing a patient’s skin, nurses should pay close attention to color, texture, temperature, and moisture. For instance, pallor may indicate anemia, cyanosis could suggest oxygen deficiency, and jaundice might point to liver dysfunction. Warmth might signal infection or inflammation, while cool, clammy skin could indicate shock or poor circulation.
Wound assessment is another essential nursing skill. Understanding the stages of wound healing - hemostasis, inflammation, proliferation, and remodeling - enables nurses to provide effective care and identify complications early. Factors like poor nutrition, diabetes, smoking, certain medications, and advanced age can impair the healing process.
Pressure injuries, caused by prolonged pressure reducing blood flow to tissues, are a significant concern. Risk factors include immobility, poor nutrition, moisture, and friction. Nurses use tools like the Braden Scale to assess a patient’s risk, evaluating factors such as sensory perception, moisture levels, activity, and nutritional status.
Skin conditions like eczema, psoriasis, and dermatitis require careful evaluation and patient education. These conditions often have triggers, such as stress, specific foods, or environmental factors. Nurses play a key role in helping patients identify these triggers and develop management plans.
The skin’s role in infection control is crucial. Intact skin acts as the body’s first line of defense against pathogens. When this barrier is compromised - through cuts, surgical wounds, or chronic ulcers - the risk of infection rises significantly. Nurses must be proficient in wound care techniques, including proper cleaning, dressing selection, and recognizing signs of infection like redness, warmth, swelling, or purulent drainage.
Aging brings unique challenges to the integumentary system. As people grow older, their skin becomes thinner, less elastic, and more fragile. Reduced natural oil production leads to dryness, increasing the risk of tears and pressure injuries. By understanding these changes, nurses can adapt care strategies and educate patients on proper skin care.
Medications can also impact the skin. Some drugs cause photosensitivity, making patients more prone to sunburn, while others may lead to rashes, pigmentation changes, or delayed wound healing. Chemotherapy drugs often affect hair growth and skin integrity, requiring specialized care and patient support.
The psychological effects of changes to the integumentary system should not be underestimated. Visible skin conditions, hair loss, or disfiguring wounds can deeply affect a patient’s self-esteem and quality of life. Nurses must address these concerns by providing emotional support and connecting patients with resources to cope.
Accurate documentation is essential. Record details like wound size, appearance, drainage, and tissue condition. When permitted, photographs can be used to monitor progress over time.
The integumentary system’s connections to other body systems become clear in various disease processes, highlighting its role as a critical component of overall health and well-being.
How Skin Color Works
10. Reproductive System
Understanding reproductive anatomy is a cornerstone of effective patient care, especially in fields like obstetrics, gynecology, and urology. For nurses, a thorough knowledge of both male and female reproductive systems is essential to provide accurate assessments, address concerns, and educate patients.
The female reproductive system is divided into external and internal structures. Externally, the vulva includes the mons pubis, labia majora, labia minora, clitoris, vestibule, and perineum. The mons pubis is a fatty area above the pubic bone that provides cushioning and contains sebaceous glands. The labia majora protect the underlying structures, while the labia minora shield the urethral and vaginal openings. The clitoris, containing over 8,000 sensory nerve endings, is a primary source of sexual pleasure and functions similarly to the male penis. The vestibule, located between the clitoris and vaginal opening, includes the urethral meatus and openings for the Bartholin glands (which provide lubrication) and Skene glands (homologous to the male prostate). Additionally, the hymen, a thin membrane at the vaginal opening, and the perineum, the area between the vaginal opening and anus, are important in childbirth assessments.
Internally, the vagina is a muscular canal approximately 7.5–10 cm long. Its rugae allow for flexibility during intercourse and childbirth, and its acidic pH of around 4.5, maintained by Lactobacillus bacteria, helps prevent infections. The uterus, an inverted pear-shaped organ about 5 cm wide and 7 cm long, is located between the bladder and rectum. It supports fetal development and plays a critical role during labor. The uterus consists of the fundus (the muscular upper part), the corpus (the main body that expands during pregnancy), and three layers: the outer perimetrium, the myometrium (responsible for contractions), and the endometrium (where implantation occurs and which sheds during menstruation). The cervix connects the uterus to the vagina, with the endocervical canal containing an external and internal os. The transformation zone near the squamocolumnar junction is a key area for cervical cancer screening.
The uterine (fallopian) tubes, roughly 10 cm long, extend from the uterus and play a role in transporting sperm to the egg and guiding fertilized eggs back to the uterus. These tubes are divided into the isthmus, ampulla (the typical site of fertilization), and infundibulum, which features fimbriae that help capture the egg. The movement of the egg is aided by ciliated epithelial cells and peristalsis. The ovaries, located on either side of the uterus and measuring 3–5 cm during reproductive years, release eggs and produce hormones. Additionally, the breasts function as accessory reproductive organs, containing mammary glands, alveoli for milk production, and lactiferous ducts that carry milk to the nipple.
The male reproductive system focuses on the testes, which produce sperm and testosterone. The testes are housed in the scrotum, which regulates temperature for optimal sperm production. Within the testes, seminiferous tubules are responsible for sperm development, and mature sperm are stored in the epididymis. During ejaculation, sperm travel through the vas deferens, which is part of the spermatic cord - a bundle that also contains blood vessels and nerves. Accessory structures like the seminal vesicles contribute a fructose-rich fluid to energize sperm, while the prostate gland, located near the rectum and surrounding the urethra, secretes an alkaline fluid that supports semen coagulation and liquefaction.
A deep understanding of reproductive anatomy enables nurses to recognize variations, address health concerns, and educate patients effectively. This knowledge is especially critical when dealing with issues like fertility challenges, sexually transmitted infections, hormonal imbalances, and reproductive cancers. Given the personal and often sensitive nature of reproductive health, nurses must approach these topics with empathy, professionalism, and cultural sensitivity. Accurate documentation and patient education are vital for ensuring continuity of care and empowering patients to make informed decisions about their health.
Thanks For Creating Me Dad… With Your Testicles
Is the G-Spot Real? Here's What the Science Says...
System Comparison Chart
These comparison charts are designed to provide a quick overview of the key differences and interactions between related systems. They complement the detailed descriptions above, helping to identify essential interconnections for effective clinical assessments.
Musculoskeletal Systems: Skeletal vs. Muscular
The skeletal and muscular systems function as a team, enabling movement and maintaining the body's stability.
| Feature | Skeletal System | Muscular System | How They Work Together |
|---|---|---|---|
| Primary Function | Provides the body's framework and shields vital organs | Produces force for movement and supports posture | Muscles contract to pull on bones, creating movement |
| Structure | Includes 206 bones, along with cartilage, ligaments, and joints | Comprises over 600 skeletal muscles and tendons | Ligaments connect bones, while muscles stabilize joints dynamically |
| Control | Passive system activated by muscle action | Voluntarily controlled via nervous system signals | Nervous system triggers muscle contractions to move the skeletal framework |
| Role in Movement | Acts as levers and provides attachment points | Contracts actively to generate motion | Muscles pull bones across joints, moving the body efficiently |
Circulatory vs. Respiratory Systems
These systems collaborate to deliver oxygen to tissues and remove carbon dioxide, ensuring the body functions properly.
| Aspect | Circulatory System | Respiratory System | Nursing Interventions |
|---|---|---|---|
| Primary Function | Transports oxygen, nutrients, and waste through the bloodstream | Facilitates gas exchange between air and blood | Monitor heart and respiratory rates together for a full assessment |
| Key Structures | Includes the heart, blood vessels, and blood | Composed of lungs, airways, and the diaphragm | Evaluate circulation and breathing as interconnected processes |
| Common Symptoms | Chest pain, irregular heartbeat, swelling | Shortness of breath, coughing, wheezing | Watch for cyanosis, which can signal issues in both systems |
| Assessment Focus | Pulse, blood pressure, heart sounds | Breath sounds, oxygen levels, respiratory effort | Use pulse oximetry to check the effectiveness of both systems simultaneously |
Digestive vs. Urinary Systems
While both systems remove waste from the body, they handle different materials through distinct processes.
| Feature | Digestive System | Urinary System | Clinical Considerations |
|---|---|---|---|
| Waste Removal | Eliminates solid waste and undigested food | Filters and excretes liquid waste and toxins | Dehydration can impair both systems significantly |
| Key Organs | Includes the stomach, intestines, liver, and pancreas | Comprises the kidneys, bladder, ureters, and urethra | Kidney dysfunction may affect how medications are processed |
| Fluid Balance | Absorbs water and nutrients | Regulates water and electrolyte levels | Track fluid intake and output for both systems carefully |
| Common Issues | Nausea, vomiting, constipation, diarrhea | Reduced urine output, painful urination, incontinence | Fluid restrictions may be needed to manage certain conditions in both systems |
Nervous vs. Endocrine Systems
These two systems regulate body functions but use different mechanisms - electrical signals for the nervous system and chemical messengers for the endocrine system.
| Characteristic | Nervous System | Endocrine System | Patient Care Impact |
|---|---|---|---|
| Communication Method | Sends electrical impulses through neurons | Releases hormones into the bloodstream | Nervous system effects are immediate, while hormonal changes take longer |
| Response Speed | Instantaneous (milliseconds) | Delayed (minutes to hours) | Rapidly address neurological changes; monitor endocrine symptoms over time |
| Duration of Effect | Short-term and precise | Long-lasting and widespread | Neurological care often requires quick action; endocrine issues need ongoing management |
| Control Functions | Manages reflexes, voluntary movements, and consciousness | Oversees growth, metabolism, reproduction, and stress responses | Collaboration between neurology and endocrinology teams is essential for comprehensive care |
Integumentary System Compared to Other Systems
The skin interacts with multiple body systems, making it a key indicator of overall health.
| System Interaction | Skin Indicators | Normal Findings | Abnormal Findings |
|---|---|---|---|
| Circulatory | Reflects blood flow and oxygenation | Pink, warm skin with good capillary refill | Cyanosis, pallor, poor circulation, or edema |
| Respiratory | Shows oxygen levels | Normal color, no nail clubbing | Blue-tinged skin or clubbing, which may indicate chronic low oxygen |
| Endocrine | Mirrors hormonal balance | Smooth skin with appropriate hair distribution | Excessive hair growth or changes linked to conditions like diabetes |
| Immune | Signals infection or inflammation | Intact skin without lesions | Persistent rashes, slow-healing wounds, or unusual infections |
The skin often provides early clues about underlying health issues. For example, changes in skin color might reflect circulatory problems, while muscle weakness could hint at nervous or endocrine system concerns. Recognizing these connections is crucial for delivering thorough patient care and catching complications early.
Conclusion
Gaining a solid grasp of the 10 body systems is essential for effective nursing practice. Understanding how these systems interact allows for more accurate assessments and timely interventions. This knowledge transforms routine check-ups into powerful diagnostic tools, helping to identify potential complications early and take action before they escalate.
The body’s interconnected nature means that an issue in one system often affects others. For example, noticing a decrease in urine output might point to kidney problems, which could also impact how medications are processed. Similarly, changes in the skin might signal concerns related to circulation, respiration, or hormone regulation. This broader perspective equips you to think critically and connect the dots, enhancing your ability to provide comprehensive care.
Modern tools like interactive courses, 3D anatomical models, and simulations have revolutionized how nurses study anatomy. While these digital resources offer engaging ways to learn, hands-on experiences like cadaver studies remain unmatched. Institutions like the Institute of Human Anatomy demonstrate how working with real human tissue provides insights into natural anatomical variations that digital models simply can’t replicate. This hands-on exposure sharpens your ability to spot subtle clinical signs - skills that can make a life-saving difference in practice.
By combining these educational tools, you not only refine your clinical skills but also set yourself up for long-term success in your nursing career. Whether you’re in emergency care, pediatrics, geriatrics, or another specialty, a deep understanding of the body’s systems empowers you to deliver safer and more effective care. Your ability to recognize small but critical changes, anticipate potential issues, and collaborate with your team directly benefits your patients.
Blending hands-on and digital learning ensures that every piece of knowledge you gain translates into better patient care. The complexity of the human body requires continuous learning, and every new insight you acquire strengthens your ability to make a real difference in the lives of those you care for.
FAQs
Why is it essential for nurses to understand how body systems work together?
A nurse's ability to grasp how body systems work together is crucial because the human body operates as a unified network. When one system - such as the respiratory or cardiovascular system - faces an issue, it often sets off a chain reaction in others. Understanding these interconnections allows nurses to spot symptoms early, foresee potential complications, and deliver more effective care.
Take, for instance, a heart condition. It can cause fluid to accumulate in the lungs, disrupting the respiratory system. With a clear understanding of these links, nurses can tailor treatments more effectively and enhance patient outcomes. This comprehensive approach is essential for providing high-quality, patient-focused care.
What are the best ways for nurses to care for patients with complex conditions like diabetes and heart failure?
Nurses caring for patients with complex conditions need a solid grasp of how different body systems work together. For instance, understanding how diabetes can influence heart failure is crucial. By closely monitoring symptoms and vital signs, nurses can spot potential problems early and address them promptly.
Providing effective care also means maintaining clear communication with the healthcare team, helping patients understand their conditions, and delivering appropriate interventions within the nurse's role. Tools like patient charts and care plans play a big part in keeping care organized and aimed at improving patient outcomes. Being detail-oriented and proactive makes all the difference.
What are the best tools and strategies for nurses to better understand complex body systems?
Nurses can deepen their grasp of complex body systems by leveraging a mix of educational resources and strategies. Tools like anatomy atlases, 3D models, and online simulations provide a clear, visual way to explore structures and their functions. Pairing these with case studies and multimedia tools - such as radiology images, animations, and quizzes - helps bridge the gap between theoretical knowledge and practical application.
To make learning even more effective, combining these resources with study guides and visual aids can reinforce critical concepts. Hands-on approaches, like interactive modules or real-world applications, not only simplify challenging topics but also make the learning process more engaging and memorable.


